ABOVE: © ISTOCK.COM, CIPHOTOS
EDITOR’S CHOICE IN DRUG DEVELOPMENT
The paper
Z. Zhu et al., “Zika virus targets glioblastoma stem cells through a SOX2-integrin αvβ5 axis,” Cell Stem Cell, 26:187–204.E10, 2020.
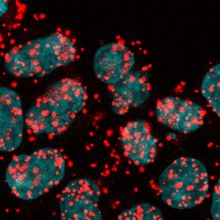
In 2017, University of California, San Diego, regenerative medicine researcher Zhe Zhu and colleagues found that the Zika virus, which sparked a widespread epidemic in the Americas a few years ago and is known to cause microcephaly in fetuses by destroying neural stem cells, preferentially targets and kills glioblastoma stem cells. The researchers argued that a modified form of Zika could potentially be used as an oncolytic virus therapy against glioblastoma, an aggressive type of brain cancer.

Following up on that work, Zhu...
Following up on that work, Zhu and collaborators set out to find “the unique property of this virus” that allows Zika to selectively target brain cancer stem cells while sparing adjacent tissues, says Zhu. Previous research has shown that a number of viruses use integrins, a group of transmembrane cell adhesion receptors, as gateways for entering host cells. The team wondered whether the same was true of Zika.
Using antibodies, the researchers blocked different integrins in brain cancer stem cells and found that the integrin αvβ5, which is produced at higher levels in brain cancer tissue than in normal brain tissue, seemed to be responsible for helping the virus enter the cells. Silencing the same integrin in a brain cancer mouse model, human brain organoids, and glioblastoma surgical samples also blocked Zika infection.
Zhu and his collaborators believe that understanding Zika’s entry mechanism can lead them closer to treatments for glioblastoma. “We hope that we can eventually use this virus in clinical trials and help to improve the outcome of the patient,” he says.
Hongjun Song, a neural stem cell researcher at the University of Pennsylvania who was not involved in the study, agrees that a modified version of the Zika virus is a potential therapeutic tool for treating glioblastoma. The approach is still a long way from clinical trials, Song says, “but this is a really interesting mechanistic study to go towards that direction.”
Amy Schleunes is an intern at The Scientist. Email her at aschleunes@the-scientist.com.
Interested in reading more?