ABOVE: © ISTOCK.COM, ELENABS
Early in the pandemic, maternal-fetal health specialists had to confront the fact that there were no easy answers they could give their patients regarding how COVID-19 might affect their pregnancies. Dani Dumitriu, a physician-scientist affiliated with Columbia University in New York, recalls that the university’s Irving Medical Center was the first hospital in the country to admit a pregnant woman with COVID-19, and as a result, “we at Columbia felt a great responsibility, being that we were the first epicenter, to generate knowledge very rapidly.”
Early questions centered around very basic aspects of the disease, including whether pregnancy increases the risk of getting sicker or dying from the virus and if it was possible to transmit the virus to a fetus in utero or to an infant through breastfeeding. When parents-to-be first began showing up to the hospital, some of them critically ill, “there was really only a little bit of literature from China” addressing questions like these, Dumitriu says, “and we didn’t know how much it would translate” to the local patient population.
Vertical transmission is not the be all and end all, and there’s many more subtle impacts that can happen on the developing fetus.
—Andrea Edlow, Massachusetts General Hospital
Years into the pandemic, some of these questions have now been answered, while others are still being fleshed out. The physical and immunological changes that take place during pregnancy do appear to make pregnant people more susceptible to severe disease, pregnancy complications such as preterm birth or miscarriages, and death. And as cohorts of children born during the pandemic pass major developmental milestones, researchers are beginning to identify possible long-term effects to SARS-CoV-2 exposure in utero. Looking back on 2020, “we know a lot more than we did then,” Dumitriu tells The Scientist. “But there are still a lot of answers we’re working towards.”
How pregnancy ups the risks that come with COVID-19
During pregnancy, the body undergoes a series of drastic physical and immunological changes to accommodate a growing fetus, and some of these changes increase vulnerability to respiratory viruses such as SARS-CoV-2. For example, pregnant people produce more blood than normal in order to sustain the placenta. To pump that blood around, cardiovascular output can increase by as much as 40 percent, leaving them more vulnerable to heart attack, arrythmias, and heart failure—conditions that overlap with COVID-19 complications. And as the fetus grows, the uterus pushes against the diaphragm, making it difficult to draw deep breaths or to cough forcefully—this is why pregnant people are generally at a higher risk for developing pneumonia, and another possible reason why COVID-19 might hit them more severely.
See “Doctors and Researchers Probe How COVID-19 Attacks the Heart”
There are also immune changes that take place throughout pregnancy to avoid an inflammatory response to the fetus and placenta. These changes take place in three phases linked to the trimesters—a so-called pregnancy immune clock—meaning that infection with SARS-CoV-2 can manifest differently depending on the timing, according to Massachusetts General Hospital maternal-fetal medicine specialist Andrea Edlow. But even with these broad overarching changes to the immune landscape, Edlow notes that “there’s not a universal truth that any trimester of pregnancy looks the same for every pregnant individual.”
Studies during the pandemic have routinely shown that pregnant people infected with SARS-CoV-2 are at higher risk for severe disease, death, and complications such as preeclampsia, miscarriages, and preterm birth compared to those without the disease, particularly when parents were infected later in their pregnancies. Like others in their age group, most infected pregnant people report asymptomatic or mild cases of the disease, but pregnant people who are admitted to the hospital with COVID-19 are more likely than their peers to spend time in the ICU and to require invasive ventilation. This has been true worldwide, with studies from China, Israel, the UK, the US, sub-Saharan Africa, and international consortiums all reporting the same broad trends (with regional differences). In pregnancy, as in the broader pandemic, minority racial and ethnic groups are more likely to experience these adverse outcomes.
As new variants have replaced older ones, these patterns have largely held. The data are still rolling in, especially for Omicron, but the preliminary consensus is that variants have resulted in more cases and sometimes, but not always, caused more severe illness than their predecessors, with Edlow calling Delta in particular a “worse actor.” In one study, scientists found that infections in pregnant people when Delta predominated were more severe than those during the Alpha wave of late 2020, leading to more incidences of pneumonia, more cases that required respiratory support, and more ICU admissions. Another paper, published in JAMA earlier this year and based on admissions to a prenatal health network in Texas during the Delta and Omicron surges, found that three times as many pregnant people tested positive for COVID-19 during the Delta surge, and 10 times as many during the Omicron surge, than during a pre-Delta period of the pandemic. Compared to the pre-Delta period, Omicron cases were about 80 percent less likely to be severe in terms of the need for interventions such as supplemental oxygen or intubation, while Delta cases were three times more likely to be severe.
With respect to pregnancy complications, severe cases of COVID-19 have been linked to placental abnormalities, preeclampsia, early miscarriages, stillbirths, and preterm births. In one study, women infected with SARS-CoV-2 later in pregnancy (after 34 weeks) were seven times more likely to report a preterm birth, while in another, which included over 1 million women, a COVID-19 infection was two times as likely to be associated with a stillbirth, regardless of the trimester of infection. Pregnant people who contract COVID-19 are also two times as likely to develop preeclampsia, which can be fatal.
See “Human Fetuses Can Contract SARS-CoV-2, but It’s Rare”
To explain these findings, several researchers have probed the mechanisms of how SARS-CoV-2 interacts with the maternal-fetal interface, a specialized tissue derived from the uterus and placenta, to influence disease. An early study published by Edlow and her colleagues, for example, found that evidence of vertical transmission—that is, transmission of SARS-CoV-2 from mother to fetus across the womb—is extremely rare, limited to just a handful of cases. However, she adds, “vertical transmission is not the be all and end all, and there’s many more subtle impacts that can happen on the developing fetus.”
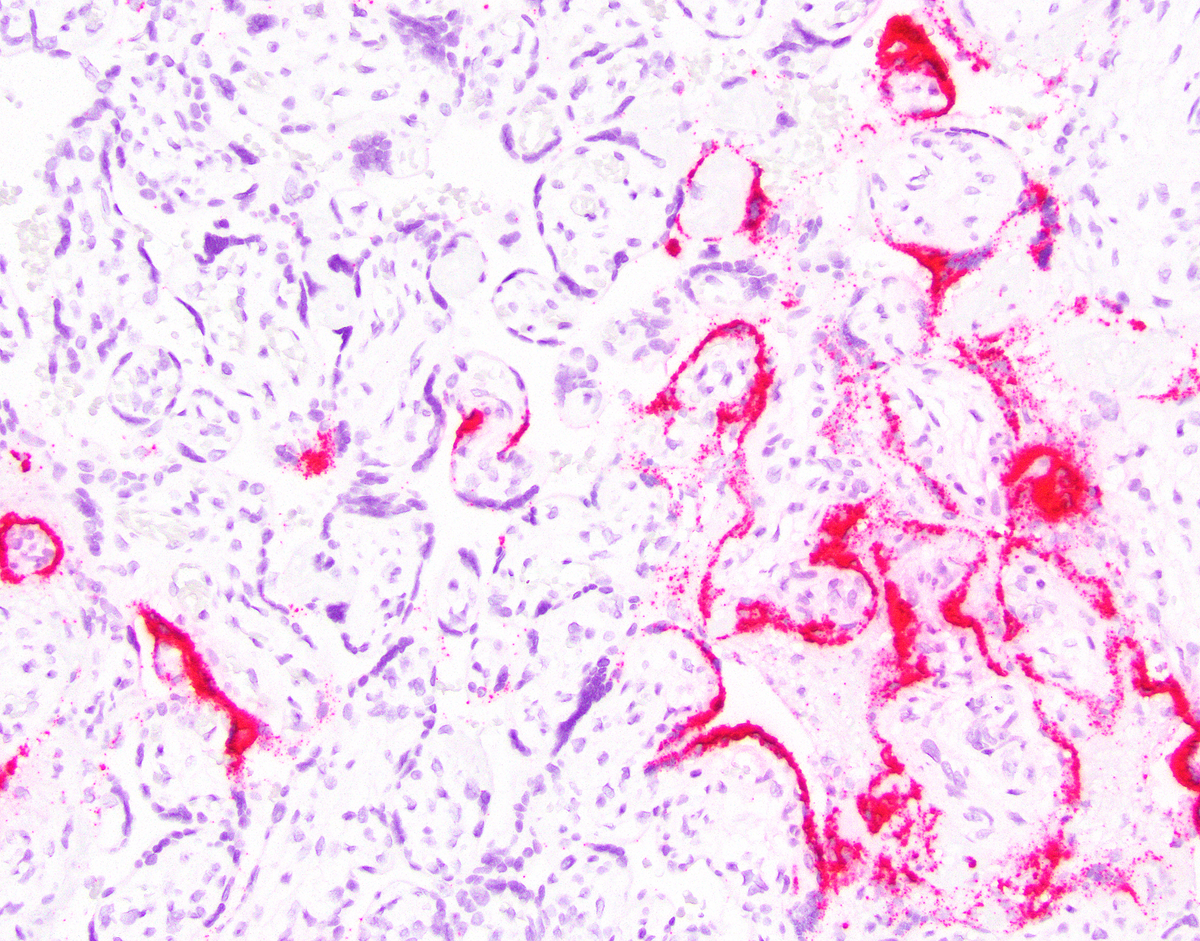
Ilhem Messaoudi, an immunologist at the University of Kentucky College of Medicine who specializes in viral diseases and maternal-fetal health, recently investigated these other effects, looking specifically at asymptomatic or mild infections. While her sample size was relatively small—just nine pregnant women with COVID-19 and 15 uninfected controls—she found that even mild infections can have a lasting effect on the maternal-fetal interface. Months after their first positive test, the women’s immune response remained shifted toward a proinflammatory state, with an increased abundance of memory T cells and a reduction in immune-suppressing regulatory T cells in the mother’s blood as well as an uptick in cytokine-secreting macrophages in maternally derived placental tissue, which was collected at birth.
“When I initially started these studies, I had this naive view that somehow the placenta was this protected organ that was made out of Kevlar or something, but clearly it’s not,” Messaoudi says. “These changes occur, they reverberate through the maternal-fetal interface, and they persist. And anytime you talk about enhanced inflammation . . . that is not without a consequence. Being bombarded by inflammation in utero is going to have a cost down the line.” Specifically, she says she wants to know whether that exposure remodels the fetus’s immune system during development such that it could change how these infants respond to childhood vaccinations.
The years to come
Some babies born during the pandemic have since celebrated their first and even second birthdays, and researchers are following these children to see whether maternal SARS-CoV-2 infection is linked to neurodevelopmental delays after birth. Based on previous disease outbreaks, scientists know that a viral challenge during pregnancy can sometimes lead to lifelong effects for the child. Cohort studies following the influenza pandemics of 1918 and 1957, for example, found that people born during the outbreaks attained lower education levels and had higher rates of schizophrenia. A rubella pandemic in 1964 was associated with a 10- to 15-fold increase in diagnoses of autism spectrum disorder and schizophrenia.
Roy Perlis, the director of the Center for Quantitative Health at Massachusetts General Hospital, recently published the results of a study assessing the neurodevelopmental outcomes at one year of age among hundreds of infants born in 2020 to mothers who tested positive for COVID-19 during their pregnancies. His team, of which Edlow is a part, found that maternal infection was associated with a greater incidence of diagnoses of disorders related to speech, language, and motor function, even when race, ethnicity, insurance status, offspring sex, maternal age, and preterm status were accounted for. The hopeful caveat, Perlis tells The Scientist, is that these are “nonspecific diagnoses,” meaning that “in many cases, they resolve on their own and don’t have any implications for the longer term. On the other hand, that’s not always the case.”
See “Sex of Fetus Affects Immune Response to COVID-19 During Pregnancy”
When Columbia’s Dumitriu looked into this same question in a cohort of six-month-old infants using a standard risk screening questionnaire, she failed to find evidence of impaired neurodevelopment following maternal exposure to SARS-CoV-2. The group has since developed an observational assessment of babies for use over Zoom, and has shared preliminary evidence at conferences that Dumitriu says “reinforces this lack of an effect of COVID infection during pregnancy on neurodevelopment.”
This virus just continually surprises people this far into the pandemic, and we don’t necessarily know what’s coming around the corner.
—Dani Dumitriu, Columbia University
Perlis says that he isn’t particularly surprised by the differences between the two studies. The two papers used different metrics to assess delays—one based on risk and the other on actual diagnoses—and it may also be that six months is too early to capture many missed milestones. “We need to look at this question in different ways, and so all of the various approaches to understanding it are valuable,” he says. “The idea was always for [our study] to be the first of a series of reports that will expand as the cohort grows and as these kids get older.” The two teams will soon assess their respective cohorts’ risk for autism spectrum disorder, and later, for conditions such as attention-deficit/hyperactivity disorder, depression, anxiety, and schizophrenia—links that took decades to become clear after past pandemics.
Although Dumitriu didn’t find an effect of COVID-19 exposure in her cohort, she did find an unexpected result when, as she was preparing to publish her initial findings, she approached one of her team members about including a group of pre-pandemic children in the analysis. Shortly after, her colleague called her in a panic, Dumitriu recalls. “She couldn’t breathe on the phone. I had to calm her down.”
The new work showed that, compared with children born before 2020, all of the pandemic babies, regardless of their SARS-CoV-2 exposure status, scored significantly lower on gross and fine motor skills and personal-social interactions, suggesting that something about being born into and growing up during the pandemic was creating an increased risk for missing developmental milestones. “On the heels of having this really incredibly good news when we were expecting a viral infection effect, it was very surprising,” says Dumitriu, who attributes the differences between pre- and post-pandemic babies to the effects of maternal stress. Her current work aims to tease apart how exactly that stress manifests and what it might mean for maternal and fetal health.
Multiple researchers stress that even as we learn more about the interplay between COVID-19 and pregnancy, there’s no space to let our guard down. New strains appear to be more transmissible, and if a future variant were to also induce higher incidences of severe disease, it could be especially troublesome for pregnant individuals. “We can’t stop investing in this research, [and] we can’t stop being vigilant,” Dumitriu says. “This virus just continually surprises people this far into the pandemic, and we don’t necessarily know what’s coming around the corner.”
Arrival of vaccinesThe availability of authorized vaccines, including those from Pfizer/BioNTech, Moderna, and Johnson & Johnson, brought up a host of new questions around the safety and effectiveness of the shots in pregnant people. Because this demographic is high-risk for complications, and because vaccine manufacturers didn’t want to be liable for unintended effects of vaccination on a developing fetus, pregnant people were omitted from many of the early clinical trials, but now those efforts are underway. Christine Olson, a physician-scientist at the US Centers for Disease Control and Prevention (CDC) who oversees the agency’s v-safe COVID-19 vaccine pregnancy registry, was part of the team that released the first preliminary data on COVID-19 vaccine safety in roughly 850 pregnant people in spring 2021. While some participants reported preterm births or bearing children who were small for their gestational age, the percentages (9.4 percent and 3.2 percent, respectively) did not significantly differ from pregnant people studied prior to the pandemic. Similarly, pregnant people were found not to be at increased risk for adverse side effects following their injections compared with nonpregnant controls. Since then, Olson says, the data have continued to support the vaccines’ safety, and the registry now includes more than 23,000 participants. “We have not detected any [adverse] safety signals in our ongoing monitoring of the data that has continued to come in over the course of people’s pregnancies and . . . during the postpartum period,” Olson says. See “COVID-19 Vaccines for Pregnant Moms May Protect Newborns”Moreover, preliminary data suggest that getting vaccinated for COVID-19 during pregnancy can confer pre- and post-birth benefits to the child. CDC epidemiologist Sascha Ellington tells The Scientist that several studies have since documented “that vaccination before and during pregnancy builds antibodies that are passed to and can help protect the fetus/infant,” including research showing that COVID-19 vaccination is more protective to both mother and baby than a natural infection. Babies born to mothers who were vaccinated during pregnancy, for example, had elevated levels of circulating SARS-CoV-2 antibodies in their blood, and researchers have detected a corresponding bump in antibodies in breastmilk from women who got a booster. Preliminary evidence suggests these antibodies are protective: A CDC report earlier this year found that maternal immunization during pregnancy was associated with a reduced risk for COVID-19 hospitalization among infants less than six months of age during a period when both Delta and Omicron were circulating. The National Institute of Allergy and Infectious Diseases (NIAID) recently launched a clinical trial called MOMI-Vax to evaluate the immune responses generated by pregnant people in response to COVID-19 vaccination. Flor Munoz-Rivas, a pediatric infectious disease specialist at the Baylor College of Medicine who is overseeing the trial, says in an email that because none of the existing vaccines are authorized for children six months and under, “understanding the potential direct (through vaccination and transplacental transfer of antibodies) and indirect (through breast milk or decreasing maternal infection risk) protection from maternal vaccination during pregnancy or post-partum is essential at this time.” |








